Located at 20 Old Brompton Road – Just Steps from ![]() South Kensington Tube. Easy Access, Always.
South Kensington Tube. Easy Access, Always.
Hpv Vaccine
What is HPV?
Human Papilloma Virus (HPV) is the UKs most prevalent sexually transmitted infection. The virus has several types, with certain types categorised as high risk because they are associated with the development of certain types of cancers.
HPV-related cancers include cervical, anal, genital cancer, and cancer of the neck and head. Other conditions like genital warts or verrucas are also linked to HPV.
About 99.7% of cervical cancer cases are as a result of contracting any of the high-risk HPV, but a large percentage of the other types of cancers are not caused by HPV. These cancers are a result of other high-risk factors like smoking and drinking alcohol.
Not all persons infected by the virus show its symptoms. Many people living with HPV do so for years without knowing.
Types Of HPV And What They Do
There are several types of HPV, about a hundred in number. About 40 out of the 100 affect genitals. The virus has a high prevalence and mostly transmitted through all kinds of sexual activities. Most people contract the virus at some point in their lives, but their bodies naturally fight and get rid of it before it causes any harm.
However, most people who contract the high-risk types of the virus are usually not able to get rid of it naturally without taking medication. Over time, a high-risk HPV infection can cause changes in the abdominal tissue which can result in cancer if left untreated.
High-risk HPV can lead to cancer of the
- Vagina
- Cervix
- Anus
- Penis
- Some cases of head and neck cancers.
Other infections like
- Genital warts which are a small growth or skin change on or around the genital or anal area,
- Skin warts
- Warts on the voice box or vocal cord (laryngeal papillomas)
How Does The HPV Vaccine Work?
The provides a vaccine called Gardasil through its national HPV vaccination programme. The vaccine protects against HPV types 6, 11, 16, and 18. Amongst these 4 types of HPV, type 16 and 18 are responsible for most cases of cervical cancer (more than 70% in the UK). They also cause a small percentage of the other types of cancer.
Type 6 and 11 of the HPV cause about 90% of genital warts. When girls are vaccinated with Gardasil, it protects them against cervical cancer and genital warts.
However, Gardasil vaccine does not protect against other types of STI like chlamydia, and it doesn't stop girls from getting pregnant. Developing and practising safe sex habits is the only guarantee against STIs and getting pregnant.
Who Can Be Vaccinated Through The Vaccination Programme?
The vaccination programme covers a wide range of people within 12 to 13 years of age. Starting from September 2019, the first HPV dose of vaccine will be routinely administered to girls and boys in school Year 8 aged between 12-13, then the second dose will be administered 6 – 12 months after the first dose (school year 8 or 9).
Those who miss either of the vaccine doses are advised to contact their GP or school immunisation team so they can complete the vaccine as soon as possible because both doses must be taken to be fully protected.
For persons who are eligible for the vaccination in school Year 8 but missed it can still get the vaccine up to their 25th birthday.
Persons who get the first dose of the vaccine after the age of 15 will need to take 3 doses of it instead of 2.
How Is The HPV Vaccination Programme Changing?
In July 2018, the announced the HPV vaccine would be extended to boys within the age of 12 and 13 in England. This decision was made to make sure many boys, in addition to girls, are offered protection against HPV from the 2019-20 school year.
This decision was based on the advice from the independent body (Joint Committee on Vaccination and Immunisation) that advises the UK health departments on immunisation.
From the 2019 - 2020 school year, boys and girls between 12 – 13 years in school Year 8 will be eligible for the HPV vaccine in London.
The extension of the HPV vaccination programme will help prevent more cases of HPV-related cancers in boys and girls.
There is no catch-up programme for older boys because evidence shows that they are indirectly protected (herd protection) from the 10 years of the girls’ HPV vaccination programme.
Why Is The HPV Vaccine Given At A Young Age?
HPV transmission can be by any form of sexual activity including touching because they are found on the fingers, hands, genital areas, and mouth. The HPV vaccine in London works better if it is given to children before they contract HPV through any form of sexual activity or become sexually active. The vaccine protects them all through their lifetime.
Individuals who are not vaccinated against the virus contract it at some point in their life, but a few are lucky to have an immune system capable of clearing out the virus while others are not so lucky. The virus stays in a dormant form in their body for many years before it causes any harm.
Women’s Health is Our Passion
Live life to the fullest with our range of Consultant-led gynaecological services.
BOOK ONLINE NOWVaccinating Against HPV For Men Who Have Sex With Men (MSM)
In the past, men who have sex with men did not benefit from the long-standing girls' HPV vaccination programme, unlike those men who have sex with women.
From April 2018, a new HPV vaccination programme was introduced. The programme allows MSM up to 45 years to be eligible for HPV vaccination on the offered in sexual health and HIV clinics in England.
HPV Vaccination For Transgender People
Trans women (people who were male at birth) are eligible for HPV vaccines in London, just like MSM as their risk of getting HPV is similar.
Trans men (people who were female at birth) are also eligible for HPV vaccination if they have sex with men and are 45 years and below.
Trans men who have previously taken the complete dose of the vaccine as part of the girls’ vaccine programme will not be eligible for the vaccination again because they are already protected.
How Is The HPV Vaccine Administered?
The HPV vaccine London consists of two injections given in the upper arm. The vaccines are given at least 6 months apart. At Gynae UK we only use Gardasil 9, which offers protection against the widest variety of HPV types.
An extra dose of the vaccine is given to people who get to take the first dose at the age of 15 and above.
MSM and transgender people who are eligible for the vaccine also need 3 doses of it.
The three doses of the vaccine are administered as follows
- Second dose- one month after the first
- Third dose- within 12 months of taking the second dose
All the doses of the vaccine must be taken properly and completed to be fully protected.
Duration Of Potency For The HPV Vaccine Protection
From several studies that have been completed, it is believed that the HPV vaccine London protects for at least 10 years, but experts expect the vaccine to last longer than what the studies show.
The HPV vaccine available does not protect against all types of HPV responsible for cervical cancer, so experts advise women from the age of 25 to have regular cervical screening whether they took the vaccine or not.
If you need more information about HPV vaccines, feel free to visit our gynaecological clinic in South Kensington, London, call us on 020 7183 5411 or send an email via info@gynaeuk.com.
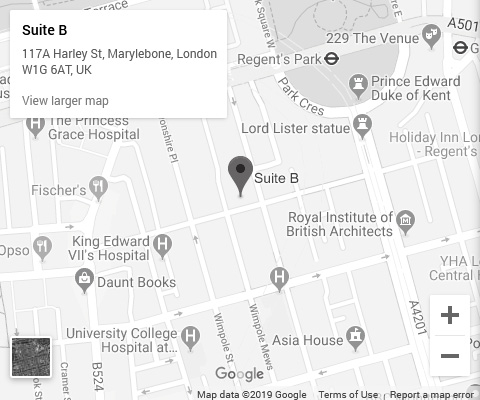 Click To View Full Map
Click To View Full Map
Contact Info
Phone: 020 71835411
Email: info@gynaeuk.com
Address:
20 Old Brompton Road, South Kensington, London SW7 3DL
Opening Hours
| Day | Opening Hours |
|---|---|
| Monday | 9am to 6pm |
| Tuesday | 9am to 8pm |
| Wednesday | 9am to 6pm |
| Thursday | 9am to 8pm |
| Friday | 8am to 5pm |
| Saturday | 10am to 4pm |
| Sunday | Closed |