Located at 20 Old Brompton Road – Just Steps from ![]() South Kensington Tube. Easy Access, Always.
South Kensington Tube. Easy Access, Always.
Menopausal health
When your regular menstrual cycle or period stops permanently, and you cannot get pregnant again, this time is described as menopause.
To some people, the time before a woman's last period is called menopause, this time is really the progression to menopause or perimenopause.
During postmenopause - the period after menopause, a woman's body has less use for the hormones progesterone and estrogen. If your level of estrogen is very low, it can affect your health and lead to symptoms like hot flushes. The good news is, you actually can do something about this to relieve the symptoms to improve your quality of life.
Basics of Menopause
Menopause is a time when your period ceases permanently. It's a normal part of your life as a woman. Sometimes, it is called 'the change of life'. Menopause is not a sudden occurrence; you may experience irregular periods and symptoms of menopause as your body transitions over the years to menopause.
What's Menopause?
If it's been a whole year since you last saw your period, then you have reached menopause. What this implies is that for 12 successive months, you've not experienced any bleeding or spotting.
At the postmenopause age, your ovaries begin to make less use of the hormones progesterone and estrogen.
What's Perimenopause?
Perimenopause means 'preceding menopause' or 'about menopause'. It is the menopausal transition or the period leading to your last menstrual cycle.
Perimenopause describes a long progression to menopause or the period when your menstrual cycle ceases permanently, and you can't conceive anymore. During this transition or progression to menopause, there will be changes in your hormone levels that will suddenly bring about symptoms of menopause. Your ovaries produce a varying quantity of the hormones progesterone and estrogen than the normal.
Also, during this time, you may have irregular periods as you may not ovulate every month as usual. You may have longer or shorter periods than you used to. For a few months, you may not see your period or experience abnormally short or long periods. Your menstrual cycle might be lighter or heavier than usual. A lot of women also experience menopausal symptoms before including hot flushes during perimenopause.
When does perimenopause begin?
The progression to menopause or perimenopause usually begins when a woman is in her middle to late 40s. On average, women experience perimenopause for 4 years before their menstrual cycle ends.
How will you know when you're having perimenopause?
It can be difficult sometimes for you and your doctor to know if you're experiencing perimenopause or the progression to menopause. But you can monitor the following:
- Irregular periods - Keep a record of your monthly periods. Irregularities in your periods may be the first sign of menopause
- Symptoms or signs - Should you have hot flushes, difficulty sleeping, or any other symptoms of menopause, consult your doctor
- Level of hormones - Should your menstrual cycle cease at an early age, perhaps before 40, your doctor may carry out a hormone test using your blood. Doctors do not usually recommend this test except on medical grounds. The reason is that, in most women, hormone levels increase and decrease unpredictably during the progression to menopause. Based on this, a blood test may not accurately tell if you've experienced menopause or the time is close by.
In what ways can menopause affect you?
Menopausal symptoms may appear at once and be very obvious, or they may be very mild initially. Symptoms may be seen most of the time or only once in a while immediately menopause sets in. Some women observe changes in a lot of areas. Some symptoms of menopause like moodiness, are similar to symptoms of premenstrual syndrome (PMS). You may not have experienced others. For instance:
- Your sex drive may become less; it may take more time for you to get sexually excited
- Vaginal dryness or irritation may become apparent as sex becomes more painful or uncomfortable for you
- You may have trouble sleeping and hot flushes
- Mood swings and easy irritation can be noticed
- Your menstrual flow may be lighter or heavier than usual
- You may experience irregular menstruation, including longer and shorter periods. You might skip some months or your period may stop for a while and then appear again.
Other signs and body changes are not so visible. For instance, your bone density can reduce because of lower estrogen levels. This could cause osteoporosis, a medical condition where bones weaken and break easily. Unstable estrogen levels can also raise cholesterol level and increase your chances of having a stroke and heart disease.
Should your menopausal symptoms be of concern to you, see your doctor for possible treatment.
How long does perimenopause last?
The progression to menopause or perimenopause can last between 2 and 8 years before your period ceases permanently. Perimenopause can last for over 4 years in most women. But you can tell whether you have reached menopause if it's been a whole year since you last had your period. This means that for 12 successive months, you've not experienced any bleeding or spotting.
Can you still use birth control during perimenopause?
Of course, yes. During the progression to menopause, whether you miss your period for only a month or a few months, you can conceive. Again, you may experience ovulation in some months during this time.
You will not be able to know accurately when your ovulation starts, so if you are not intending to get pregnant, go ahead with the use of birth control until one whole year after your last period. Consult your doctor if you need help with birth control.
After menopause, you cannot get pregnant, but should you have sex, you still stand at risk of contracting sexually transmitted infections (STIs). In a case where you have multiple sex partners, use a condom or dental dam to protect yourself when you have oral, anal, or vaginal sex. You are more prone to getting an STI from unprotected sex after menopause. This is because vaginal irritation or dryness, which is very common after menopause can cause minor tears and cuts during sexual intercourse, making you more vulnerable to infection.
At what time does menopause start?
Menopause is defined as when you've not had a period in 12 successive months. The age bracket for women is usually 45 to 58 years. You may be able to tell roughly when you'll have menopause if you know the age your mother got hers.
Early menopause can start if:
- You've never had children - If you get pregnant, especially more than once, it can delay menopause
- You smoke - Women who smoke can have menopause up to 2 years earlier than women who don't smoke
Some health issues are also associated with early menopause.
It is common for menopause to start on its own. But you can have early menopause if you've had surgery or chemotherapy to remove both ovaries. Find out more about early menopause as you read on.
After menopause, what next?
Once you experience menopause, you can no longer have a baby or see your period. Should you experience any vaginal bleeding after menopause, see your doctor immediately.
Bleeding in the vagina after menopause is abnormal and could be a sign of a severe underlying health issue.
You might notice the following after menopause:
- Vaginal dryness or irritation - A common postmenopause symptom is vaginal dryness
- Menopausal symptoms in place of menstrual issues - Postmenopause period is a time when most women are relieved of menstrual problems or menopause symptoms. But, you may go through symptoms like hot flushes due to change in estrogen level. Research shows that hot flushes can happen for about 14 years after menopause
- Fewer hormone levels - Your ovaries will produce very low estrogen and progesterone during menopause. As a result of this change in hormone level, you may be at higher risk of certain health issues like stroke, heart disease, and osteoporosis.
Symptoms and Relief of Menopause
As you grow older and approach menopause, especially during the perimenopause stage, the change in hormone levels could affect your period and lead to symptoms such as difficulty sleeping and hot flushes. With time, you may identify other symptoms like irregular menstruation, urinary issues, and pain during sexual intercourse. Consult your doctor or healthcare provider for help with your symptoms. Other forms of treatment and medicine can be of help to provide relief.
Menopausal symptoms
They include the following:
Hot flushes
The most common menopause symptom is the hot flush. 3 out of 4 women have hot flushes. Even before menopause, some women experience hot flushes whilst still menstruating.
Hot flushes are an unexpected feeling of heat around the upper body region. When you have hot flushes, your face and neck may turn red. On your arms, back, and chest, red blotches may be seen. You also get to sweat profusely during hot flushes or experience cold chills after the hot flushes. Rather than hot flushes, some women get more cold chills or flushes.
It is very common for women to have hot flushes in the year before and after their period ceases. But recent research has shown that hot flushes can be felt for about 14 years after menopause. There's no established reason why hot flushes are very common in women during menopause. Some hot flushes can be prevented using medications, and there are other ways you can get relief from hot flushes when they occur.
How to get relief
- Try using hormones - Ask your doctor for low-dose hormonal birth control if you're still having your period as this may manage your symptoms. But if you've already had menopause, then menopausal hormone therapy will be just fine. It helps relieve hot flushes and night sweats. Consult your doctor before using menopausal hormone therapy as it has associated risks. However, if you choose to use it, take it for the shortest possible time and in the lowest dose that controls your symptoms
- Try other medicines - When hormone treatment does not work for you, ask your doctor or healthcare provider for prescription drugs used for other health issues. Some medications like blood pressure medicine, epilepsy medicine, and antidepressants could alleviate hot flushes whether or not you have these health issues.
- Keep a record of your hot flushes - Note down what sets off your hot flushes and avoid them as much as you can. Some of them may be spicy foods, alcohol, a hot environment, or caffeine
- Take cold water - Have ice water at hand to drink when a hot flush is starting
- Remove a layer of clothing - As much as you can, wear clothes in layers so you can take them off when you have hot flushes
- Make use of a fan - A working fan by your bedside at night will help. If possible, keep one at work too
- Lose weight - For obese women, hot flushes may be more serious. Losing weight can be a source of relief from hot flushes
Vaginal problems and infections
As you approach menopause, the production of less amount of the hormones progesterone and estrogen will cause your vaginal tissue to get more dry and thinner.
Consequently, vaginal problems like a burning sensation, itching, discomfort, and pain may start. Sex may even become painful at this stage due to minor tears and cuts in your vagina since it's dry. You are likely to have an STI because of vaginal tears or cuts.
How to get relief
- Consider vaginal lubricant - Using a water-based, over-the-counter vaginal lubricant before or during sex can make it more relaxing for you
- Try vaginal moisturiser - You can use an over-the-counter vaginal moisturiser to lubricate your vaginal walls and make sex more enjoyable. It can be used every few days
- Prescription medicine - Discuss with your doctor on other ways to find a remedy to your vaginal dryness. This may include menopausal hormone therapy, hormonal birth control, or a prescription estrogen gel, cream, or ring that's inserted into the vagina. Since all medicine comes with risks, seek your doctor's advice first. Read on to know more about the treatment of menopause
Irregular menstrual cycle or bleeding
You may see your period less or more often. They may appear for fewer or more days and can be heavier or lighter. That you missed a couple of periods does not mean that you are experiencing the progression to menopause or perimenopause.
How to get relief
- Visit your doctor to be sure that there isn't any underlying cause of your missed periods, such as health issue or pregnancy
- Do well to see your doctor if you don't see your monthly cycle for a full year, yet you notice bleeding or spotting. For women who have experienced menopause, spotting or minor bleeding may be as a result of cancer or other major health issues
Sleeping Difficulty
Sleeping at night is difficult for most women in menopause. With low levels of the hormone progesterone, it becomes harder to fall asleep. Low estrogen levels can also result in hot flushes that cause you to sweat during sleep. It is often referred to as night sweats. Frequent urination at night is one of the symptoms a lot of women in menopause experience. Unusual tiredness during the day is another symptom.
How to get relief
- Avoid eating, drinking alcohol, or smoking before bedtime - Try not to eat rich food, smoke, and drink alcohol before you sleep. Also, stay away from caffeine after midday
- Exercise - For good night sleep, get routine physical activity. However, you should work out earlier in the day because excess activity before bedtime can keep you awake at night. Exercising during menopause will improve your night rest even if you've not been exercising regularly in the past. Research reveals that physical activities like stretching and yoga can prove to be a relief for hot flushes
- Take warm drinks - Drinking liquids like warm milk, or caffeine-free tea before going to bed can help
- Reduce screen-time close to bedtime - Reduce your use of phone, computer, or TV when it's close to bedtime, especially in your bedroom. This is because the bright light of the screen signals your brain to stay awake instead of sleep
- Adopt good sleeping habits - Learn to keep your bedroom quiet, cool, and dark. If you can, use your bedroom for sleep and sex only
- Avoid daytime naps - Practice going to bed and getting up at the same time daily
- Train your brain - Should you wake up in the night and can't sleep anymore, try doing something that will make you comfortable and fall asleep again
- Consult your family doctor - Discuss your inability to sleep with your doctor or healthcare provider, since it may be something serious. Most women develop insomnia and treating sleep problem can be a relief from severe pain
- Try treatment for hot flushes - See your doctor or healthcare provider for treatment of hot flushes should you be unable to sleep. This could help a great deal
- Treat bladder issue - If you are having bladder incontinence, don't feel it is associated with ageing. Talk to your doctor about the treatment that can help
Memory Issues
You may be forgetting things easily or unable to focus more. About two-thirds of women experiencing perimenopause report that they have issues with focusing or memory. Keep in mind that menopausal hormone therapy is not a treatment or prevention of memory loss or brain disease, including Alzheimer's disease and dementia. Recent research has shown that memory issues were part of depression and lack of sleep, but not linked to the hormone estrogen levels.
How to get relief
- Eat healthy, exercise, sleep well and quit smoking. This could boost your memory.
- Make your life socially active by joining a group or club that does activities you love, for instance, hiking. Interacting with other people in a group may aid the delay of memory loss and prevent dementia and Alzheimer's disease.
- Keep your mind active. Your mind can be improved when you concentrate on carrying out mental activities like learning a new language, taking a class, or crossword puzzles.
- See your doctor for advice should forgetfulness or other mental issues disturb your life.
Urinary issues
A lot of women go through urinary or bladder problems in menopause. The urethra may become weak from lower estrogen levels. Most women cannot contain their urine; a condition known as urinary urge incontinence. You might pee a little in your undergarments when you laugh, cough, or sneeze. This condition is known as urinary stress incontinence.
Some women going through menopause do not get enough sleep because of the number of times they wake up at night to urinate. Keep in mind that urinary issues after menopause are not associated with ageing and it can be treated.
How to get relief
- In treating urinary incontinence, you may have to limit or avoid caffeine, take medicine, use special medical devices, physical therapy, or have surgery, depending on what is causing the problem
- Urinary incontinence products like a urethra cap, pads, or a pessary can be of help if you are leaking urine. A urethra cap is a reusable product that fits over your urinary opening. A pessary looks like a round disk that can go inside your vagina to support the bladder. Your doctor will help you insert your pessary, but you can always take it out, wash, and put it back inside on your own
- Discuss with your doctor or healthcare provider things you can do at home, which can treat your urinary incontinence. Some of them may include kegel exercises (a unique type of exercise for your pelvic floor muscles). Weight loss may also be recommended as excess weight adds pressure to your nearby muscles and bladder
Mood swing
You may get easily irritated or experience crying spells. Should you have a mood swing during your menstrual cycle or depression after child delivery, you may likely have mood swings with menopause as well. But even if you never had mood swing as you go through your menstrual cycle or after childbirth, you might still experience mood swings during menopause. Again, mood swing at this stage could come from tiredness, family changes, or stress. Mood swings are not similar to depression.
How to get relief
- Get as much as 7 to 8 hours of sleep every night
- Engage in activities to feel your best; find more ways to do this
- Do not engage in so many duties as much as you can. Seek other positive ways to relieve your stress
- Join a support group in your area or online with other women experiencing menopause
- Speak with your doctor or healthcare provider about menopausal hormone therapy as this can improve mild mood swings. Every medicine has associated risks, including menopausal hormone therapy. If your mood changes during menopause, it is not the same as depression. Depression is a serious problem that needs different treatment
Anxiety and Depression
At perimenopause, your chances of anxiety and depression are higher. This could be as a result of menopausal symptoms, changing hormones, or both. It is quite natural to be depressed or sad over the loss of fertility or the body changes you are going through. Should you have symptoms of anxiety or depression, do well to see your doctor. He/she may recommend medicine, therapy, or both as a treatment for anxiety and depression.
How to get relief
- Reduce alcohol intake - Lower your alcohol consumption if you do take alcohol. The moderate daily amount of alcohol for women is one drink, and seven drinks a week. Taking more than 4 drinks at once is regarded as binge drinking
- Sleep - Get enough sleep as much as possible. Many adults need 7 to 8 hours of sleep every night. Sleeplessness is associated with depression
- Exercise - Spend a minimum of 30 minutes on most days for physical activity. Exercise improves depression
- Reduce stress - Cut down on your daily activities that can be energy-sapping. Seek good ways to relieve daily stress. You can try reading a book, relaxation techniques, spending some quiet time outdoors, or any other healthy way to ease stress
Change in sexual feeling
Menopause has different sexual effects on women. While some women may feel more comfortable, others may feel less sexually excited. You might find sex unexciting if it is painful or uncomfortable. This could be as a result of a thinner or drier vaginal wall.
How to get relief
- Should you be considered about vaginal dryness, try safe, over-the-counter and prescription treatments to enhance your vaginal lubrication. Read on to know more about menopause and your sexuality
- Some women lose interest in sex during menopause due to symptoms like anxiety, sleeplessness, or depression. Discuss with your doctor or healthcare provider about possible treatment should your menopausal symptoms be of concern
How Do You Relate Your Menopausal Symptoms To Your Family And Friends?
A lot of women going through menopause may draw support from understanding family members or friends. In case you're finding it hard to discuss menopause:
- Bear in mind that you are not the only one. All women experience menopause after a particular age
- Open up about your menopausal symptoms
- Talk about your personal experiences and ask questions
Discussing with family and friends can make them comprehend the effect menopause has on you. It might surprise to know that they may have ideas and tips that can help you.
At What Time Should I Talk To My Doctor About Menopausal Symptoms?
Should your menopause symptoms give you concern, discuss with your doctor or healthcare provider. Some of the treatment discussion may include:
- How your symptoms give you concerns
- Your age-related health risks
- If you've had a treatment like menopausal hormone therapy in the past
- If menopausal hormone therapy is ideal for you as regards your medical history
- If you are experiencing postmenopause and how long it's been ongoing
Women’s Health is Our Passion
Live life to the fullest with our range of Consultant-led gynaecological services.
BOOK ONLINE NOWTreatment of Menopause
A lot of women do not require treatment for their symptoms of menopause. You might come to realise that your symptoms disappear on their own, or your symptoms may not be uncomfortable. Should your symptoms give you concern, consult your doctor or healthcare provider to help you with relief methods. You can discuss with your medical team to get the right treatment for you. For some women, a change in eating habits and getting more exercise helps a lot. Other women may have to use medicine to get relief from their symptoms.
Are there medicines that treat menopausal symptoms?
Yes. If you are concerned about your menopause symptoms, see your doctor or healthcare provider. They can recommend medicines to alleviate your symptoms. All medicines come with risks, and your doctor could be of help to know what medicines are suitable for you.
- Low-dose hormonal birth control might be of help if you're experiencing perimenopause. These medicines can terminate or lower hot flushes, mood changes, and vaginal dryness. They can also fix heavy or irregular menstrual cycle. If you smoke, do not use hormonal birth control. This is because hormonal birth control, especially combination birth control pills and other kinds of combination birth control such as skin patch or vaginal ring may increase your risk of high blood pressure and blood clots, and for women who smoke, the risk is even higher.
- Menopausal hormone therapy aids in the treatment of symptoms of menopause when you're done with menopause. But it could increase your chances of getting a stroke, certain cancer types, and blood clots. Should you choose to use menopausal hormone therapy, take the lowest dose for the shortest possible time that ease your symptoms.
- Two non-hormonal medicines: It has been approved by the Food and Drug Administration (FDA) and may be good for the treatment of some menopausal symptoms. One low-dose selective serotonin reuptake inhibitor (SSRI), a kind of medicine normally used in treating depression, is recommended to treat hot flushes in women who have no existing anxiety or mood changes. A drug that works like estrogen in the body is approved for use in treating uncomfortable sex brought about by menopause. Discuss other FDA approved medicines for anxiety and depression with your doctor as they might help you get through symptoms of menopause.
- Menopausal hormone therapy pill or patch could treat serious vaginal dryness or discomfort
- Over-the-counter products may help if you have vaginal dryness, pain, or discomfort. A water-based vaginal lubricant could make sex less painful. Or a vaginal moisturiser can moisten the vaginal walls and cause you to enjoy sex.
- Some prescription medicines might aid in reducing vaginal pain, dryness, or discomfort if over-the-counter products are not effective. They include estrogen tablets, creams, or rings that you insert in your vagina.
- A hormonal medicine that has the generic name of prasterone is an FDA approved drug that treats women with vaginal dryness which causes pain during sexual intercourse. The drug is used on the vagina once daily.
What's menopausal hormone therapy?
This is a medicine that is prescribed to treat your menopausal symptoms such as vaginal dryness, and hot flushes if they are so serious as to make your daily life uncomfortable. Another name for menopausal hormone therapy is hormone replacement therapy or hormone therapy.
When you go through menopause, your ovaries produce little levels of the hormones progesterone and estrogen. Menopausal hormone therapy puts back some of the hormones that are lost with artificial estrogen and progesterone.
Symptoms of menopause like hot flushes and others can be treated with menopausal hormone therapy. The dosage is one pill daily. You may also get estrogen or estrogen plus progesterone menopausal hormone therapy in the form of a skin patch. Menopausal hormone therapy, just like every other medicine, has risks. Should you choose to use it, take the lowest possible dose within the shortest time.
Topical hormone therapy, a type of menopausal hormone therapy does not treat hot flushes but can relieve vaginal dryness or irritation. There are several other brands of menopausal hormone therapy.
What's topical hormone therapy?
This is a low-dose estrogen cream directly applied to the vagina. It helps with vaginal dryness but may not aid in the relief of other symptoms like hot flushes. It also comes in the form of a vaginal ring, gel, and insert. Topical hormone therapy has its own risk, which varies from that associated with hormone replacement therapy.
How safe is menopausal hormone therapy?
Menopausal hormone therapy or hormone replacement therapy is safe for use in some women but comes with risks. Which is why the FDA advises women who decide to use this medicine to do so by using the lowest possible dose effective for the shortest period needed.
Research reveals that:
- Menopausal hormone therapy lower symptoms of menopause like moodiness swings, vaginal dryness, difficulty sleeping, and hot flushes
- Using only estrogen and estrogen plus progesterone increases the risk of stroke and blood clots in the lungs and legs. For women between 50 and 59, this risk is not common
- Topical vaginal estrogen may provide relief for women suffering from vaginal discomfort or dryness during sex
- Hot flushes or flushes usually need increased doses of estrogen therapy which affects the entire body
- Menopausal hormone therapy might be an option for women who are 59 years old, but usually only within 10 years of menopause. Much younger women and others that are almost nearing the end of their period are not so susceptible to the adverse side effects of menopausal hormone therapy.
Who's not qualified for menopausal hormone therapy?
It may not be safe for certain women to undergo menopause or hormone replacement therapy. Talk to your doctor about your risks should you have:
- A family history of gallbladder disease
- Liver disease
- A history of blood clots or stroke
- Increased levels of triglycerides (a kind of fat in the blood)
- A personal or family history of breast cancer
- A history of heart disease or associated factors like high cholesterol levels
What's the duration for taking menopausal hormone therapy?
The FDA recommends that women take only estrogen or estrogen plus progesterone menopausal hormone therapy at the lowest possible dose effective within the shortest period.
Consult your doctor or healthcare provider to analyse the risks and benefits of menopausal hormone therapy considering your age, risks factors, and symptoms.
What's bioidentical hormone therapy?
This describes products that are just the same as natural hormones. The term 'bioidentical' is suggested by the companies that produce these medicines. Most of these companies also push forward the notion that their products come with more safety than menopausal hormone therapy. But the FDA does not regulate these products or recognise this term. There hasn't been any research to validate the safety or effectiveness of these products.
Consult your doctor or healthcare provider before taking any bioidentical hormone therapy.
Early or Premature Menopause
Any menopause that occurs before the age of 40 is known as premature menopause. Menopause that occurs between the ages of 40 and 45 is early menopause. Up to 5% of women experience early menopause naturally. Other habits like smoking and some medications can trigger early menopause as well.
Difference between early and premature menopause
Menopause is said to be early when the ovaries cease the production of hormones and menstrual periods stops earlier than normal. This could be a natural occurrence or a medically-induced activity as in when both ovaries are taken out in a hysterectomy.
The same thing may be responsible for early and premature menopause. The difference is the age at which it occurs. When menopause sets in before the age of 45, it is known as early menopause. Menopause happening before age 40 is known as premature menopause.
Women who have experienced early or premature menopause cannot conceive.
Causes Of Early And Premature Menopause
Early or premature menopause may occur by itself for no apparent reasons, or due to certain medications, health conditions, or surgeries. However, some causes of early or premature menopause include:
- Smoking Smoking can make women reach menopause two years earlier than those who don't smoke. Severe symptoms of menopause is another risk that women who smoke stand to get. Recent studies show that women going through early or premature menopause with the habit of smoking dies about two years earlier than women who do not smoke.
- Surgery To Take Out The Uterus Certain women who undergo a hysterectomy, an operation that removes the uterus can retain their ovaries. Should this be the case, you can no longer have monthly periods nor get pregnant. However, menopause will not begin immediately because your ovaries will still be producing hormones, but in time, you might develop natural menopause a year or two earlier than usual.
- Surgery To Take Out The Ovaries Bilateral oophorectomy, an operation that removes the two ovaries may trigger menopause immediately. You cease to get your menstrual cycle after this surgical procedure. Your hormone levels will reduce at once, and you may experience intense menopausal symptoms such as hot flushes and lower libido (sexual desire).
- Chemotherapy Or Pelvic Radiation Treatment For Cancer If you have these treatments, there may be damage to your ovaries, and your period can stop permanently or just for a little time. You could also have difficulty getting pregnant or may not be able to conceive anymore. Although it is not every woman that goes through radiation or chemotherapy that will experience menopause. Younger women who undergo chemotherapy have lesser chances of experiencing menopause.
- Family history If you come from a family with a record of early or premature menopause, you are most likely to experience it too.
Other Health Conditions
- Missing Chromosomes Women with missing chromosomes or issues with their chromosomes can experience early menopause. For instance, women with the condition known as Turner's syndrome are given birth to without all or a part of the X chromosome, as such their ovaries are not formed generally during childbirth, and their period plus perimenopause might not be the usual.
- Chronic Fatigue Syndrome Any woman with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) mostly have a very severe headache, amnesia, muscle and joint pain — weakness, tiredness, and other symptoms. Studies have revealed that women carrying this syndrome are prone to experience early or premature menopause.
- HIV And Aids HIV infected women that do not control the virus with medicine may have early menopause. They may also have severe hot flushes than those without HIV.
- Auto-Immune Diseases Like Rheumatoid Arthritis And Thyroid Disease It rarely happens anyway, but sometimes the immune system whose function is to protect the body from diseases might mistakenly fight the ovaries and stop them from producing hormones.
How To Know When You are Experiencing Early Or Premature Menopause
Of course, you know that going for 12 successive months without menstrual periods shows that you have gone through menopause. Should you suspect that you are experiencing early menopause, see your doctor or healthcare provider immediately.
- Your doctor or healthcare provider will look at your symptoms, including irregular periods, difficulty sleeping, vaginal dryness or discomfort, and hot flushes.
- Your doctor or healthcare provider may recommend a blood test to measure your estrogen and other hormone levels, such as follicle-stimulating hormone (FSH). You might want to get tested to know your chances of conceiving. During the first few days of your period, your doctor will also examine your hormone levels.
Effects Of Early Or Premature Menopause
Early menopause presents symptoms or health issues similar to that of typical menopause. Some women with premature or early menopause may experience:
- Increased risk of severe health issues, like heart diseases and osteoporosis, and women will stay alive more without the health benefits of increased estrogen levels. Consult your doctor or healthcare provider about ways to reduce your risk for these health issues.
- Extreme menopause symptoms. See your doctor or healthcare provider for treatment to alleviate the symptoms if they are of great concern.
- Depression or sadness over body changes or the early loss of fertility, you should see your doctor if you have symptoms or signs of depression, including lack of interest and excitement about the things that used to thrill you.
Based on your doctor's recommendation, you may be referred to a gynaecologist who can help you work on your feelings. Your doctor or healthcare provider can also suggest options like adoption or donor egg programs if you still like to be a parent.
Menopause and Your Health
The changes that perimenopause brings might make you more vulnerable to some health issues. Lower levels of estrogen and other age-related changes like weight gain in your body can cause more susceptibility to stroke, osteoporosis, and heart disease.
Menopause Vs My Health
In postmenopause, your ovaries produce low levels of estrogen. Of course, women who have experienced menopause do have shallow estrogen levels — it could heighten your risk of some health issues after menopause. As you age gradually, other age-related health problems may come naturally.
Some examples of the common health challenges in postmenopause are:
- Oral Problems After menopause, you may develop the tendency to have dry mouth plus an increased risk of cavities. It is a prevalent issue linked with postmenopause age.
- Urinary Incontinence Up to half of the women in their postmenopause age find it difficult to contain their urine. Low estrogen levels might cause the urethra to grow weak.
- Stroke After the age of 55, your chances for getting stroke increases two times every decade because of the low level of estrogen in your body, it could contribute to the rise in cholesterol on the artery walls leading to the brain.
- Osteoporosis The presence of very little estrogen in postmenopause may result in loss of bone mass more quickly than before, which presents a risk of getting osteoporosis — this is a medical condition where your bones go weak and break easily. Recent research has proved that women with severe hot flushes and night sweats during perimenopause usually experience more bone loss and stand a higher chance of having hip fractures than women who have less severe symptoms.
- Heart Disease Unlike men, women have a lower risk of heart disease before the age of 55. The function of the hormone estrogen is to relax blood vessels, open and help the body keep a healthy balance of bad and good cholesterol. When there is no estrogen, cholesterol may start spreading on artery walls leading to the heart. At the age of 70, women already have the same risk of heart disease as men of their age.
- Lead Poisoning Exposure to lead is not good — it stores up in the bones over time. Since the bones become weaker immediately after menopause, the lead can leak into your bloodstream. Older women can have a whopping 30% of lead in their blood than before they got to menopause. Lead in the blood increases your risk of high blood pressure and atherosclerosis (sometimes known as hardening of the arteries). This lead can make your kidney dysfunctional. It also has symptoms like that of dementia, affecting your memory and the ability to think.
Can Hormone Therapy Prevent Health issues During Menopause
No, it doesn't. Menopausal hormone therapy works on your menopause symptoms like hot flushes and vaginal dryness. Hormone replacement therapy might increase your risk for stroke, certain cancers, and blood clots. It doesn't prevent dementia or heart disease.
After Menopause What Screening Do You Need?
Every woman certainly needs routine checkups and screening tests throughout their entire life. Many women can practice safe health with:
- Regular mammograms after the age of 50 through age 75
- Regular Pap tests, even in postmenopause. Go for a Pap and HPV test every five years — if you have had a cervix until you get to the age of 65 and have undergone three clear successive tests.
- Cholesterol, blood pressure, and any other tests recommended by your doctor
- Urine, blood, and other screening tests to check for heart disease and diabetes
- Regular height measurements to know whether there is a reduction in height due to bone loss
Consult your doctor or healthcare provider for flu shots and other vaccines for shingles, pneumonia, and other ailments.
You may have to do other tests recommended by your doctor, depending on your state of health and other specific issues like urinary incontinence.
Ways To Stay Healthy During Menopause
Various things can be done for you to stay healthy and active during menopause. Some of them include:
- Quit smoking One important thing you can do to stay healthy is to stop smoking. Smoking can harm you in several ways, including causing bone damage, heart disease, and create as many as 12 types of cancer in women. Avoid secondhand smoke and seek for help quitting should you need it.
- Stay Active Regularly getting a minimum of 30 minutes exercise on most weekdays can do the magic of keeping you healthier. Physical activity can improve your mood, heart, and bones. You don't have to do complicated exercises — try brisk walking and regular household chores. Seek your doctor's advice on what activity is best for you. Set an objective of doing moderate aerobic exercises and vigorous aerobic exercises at different time intervals — you can even combine both. Partake in activities that build your muscle strength twice every week. You can also get a free exercise guide and other clues for older adults on Go4life from the National Institute on Aging at NIH website.
- Eat Healthily You still need all that fibre, vitamins, minerals, and all that essential nutrients even as you grow older. Although older women do not need too many calories. Ask your doctor to tell you your daily need for calories based on your height, weight, age, and level of activity.
- Speak With Your Doctor About Supplements Women above 50 need 2.4 micrograms of vitamin B12 and 1.5 milligrams of vitamin B6 every day. Visit your doctor to know if you will need a dietary supplement.
- During postmenopause, your calcium intake should increase. Doctors recommend that women aged 51 and above get 1,200 milligrams of calcium per day — vitamin D is also vital for healthy bones. It is also doctor's recommendation that women between 51 - 70 get 600 international units (IU) of vitamin D per day, and women aged 71 and above get 800 IU of vitamin D per day. Visit your doctor or healthcare provider, if you need vitamin D or calcium supplement.
- Have safe sex It is true that after menopause, you can no longer get pregnant, but you can still contract an STI — always use a condom or dental dam whenever you have oral, anal, or vaginal sex. It will prevent STIs. Also, your vagina may become drier and thinner after menopause, causing small cuts and tears during sexual intercourse. It can raise your risk of having STI.
After Menopause, Will I Gain Weight?
Just maybe you will. A lot of women gain an extra 5 pounds on average after menopause. Reduced estrogen levels may contribute to weight gain after menopause. However, weight gain can come as a result of your body's metabolism reducing as you grow older — you may not be physically active or eat healthy as you used to in your younger days. Muscle mass is also lost with age.
Gaining weight can put you at higher risk of cholesterol, diabetes, stroke, high blood pressure, and heart attack. The risk increases if you are obese or not eating healthy nor active.
One way to lose weight if you are obese is to consume small amounts of calories daily. Practice regular exercise and physical activity for a healthier life, but it works better to keep weight off than it does to lose it. Researchers feel that those who are physically active tend to be more hungry. So, to maintain a healthy weight, eat healthily and exercise for 30 minutes minimum a day.
Menopause and Sexuality
As you approach menopause, your sex life may change. For some women, sex becomes more enjoyable. For others, it becomes less exciting; they do not even think about it. Reduction in the hormone estrogen levels causes your vaginal to become drier and thinner. There is an available treatment that can alleviate your symptoms.
Effects Of Menopause On Your Sex Life
You may or may not experience any changes in your sex life as a result of menopause. But if you do, it may be as a result of some or all of these:
- Changes in emotion can cause stress or easy irritation
- Sweating at night could disturb your sleep and cause tiredness
- Low-level estrogen may reduce your libido (sex drive), and you may take more time to get sexually excited.
- Low-level estrogen can cause your vaginal to become drier and thinner; the condition is known as vaginal atrophy — it makes sex painful or uncomfortable.
Losing interest in sex as you age is not a medical condition that needs treatment. Should you be concerned about changes in your sexual health, talk to your doctor or healthcare provider. They can provide treatment for vaginal dryness.
Ways To Improve Your Sexual Health Before And After Menopause
Steps to improving your sexual life in perimenopause and postmenopause include:
- Don't do alcohol and drugs: These things can lower your body metabolism and stimuli
- Quit smoking: Smoking can reduce the flow of blood to the vagina and the effect of estrogen — this kills the sexual
- Be active: Regular physical activity may improve your appearance, mood, and enhance your energy level. And all these things can help you be more into sex.
- Have regular sex: Should you choose to have sex, it can cause more blood to flow to your vagina and maintain healthy tissues.
- Do more foreplay: Give more time to get aroused. The moisture that comes from arousal protects your vaginal muscles and make sex pleasurable
- Don't use products that irritate your vagina: Strong soaps and bubble baths may bring about irritation. Talk to your doctor or healthcare provider if you notice vaginal irritation or itching because it could be a symptom of infection.
- Perform pelvic floor exercises - Physical activity like kegel exercises can force more blood to the vagina and strengthen the muscles used in orgasm
- Consult your doctor or healthcare provider for products that can boost your sexual urge: Should you be concerned about your loss of interest in sex, see your doctor. Some women use products such as creams or pills with the makeup hormone testosterone or other similar products. The FDA has not approved these products for the treatment of low female libido — except flibanserin, a medicine that treats low sexual drive. Do not take alcohol if you are on flibanserin. It has severe risks of low blood pressure and unconsciousness. Flibanserin may increase your sexual pleasure by once a month or every two months. See your doctor or healthcare provider for the risks and benefits of using any medicine.
Treating Vaginal Dryness After Menopause
To take care of vaginal dryness that makes sex uncomfortable:
- Get an over-the-counter, water-based vaginal lubricant for use during sex
- Use an over-the-counter vaginal moisturiser to aid moisture production. You may need to use it very often.
In cases where the vaginal dryness is too much, your doctor may recommend some medicines you can put inside your vagina to boost moisture and pleasure including:
- A non-hormonal drug known as ospemifene
- Estrogen rings or tablets that can be inserted in the vaginal
- Vaginal estrogen creams
Visit your doctor or healthcare provider to explain your health problems and symptoms. They can recommend one or more treatments that are suitable for you.
Ways To Tell Your Partner About Menopause And Sex
Discussing your concerns with your partner can boost your relationship. As you age, severe heart disease or diabetes can affect your sexual health and sex drive. Talk to your partner about things like:
- What feels good and what doesn't
- When you might be more relaxed
- More comfortable positions
- If you need more time for foreplay to increase arousal
- Concerns about changes in your appearance
- Other ways to pleasure each other aside vaginal sex, like oral sex and hot massage
You could book an appointment with a therapist or sex counsellor for private therapy if you are concerned about changes in your sex life. You may also go with your partner to this appointment.
Is Safe Sex Still Important After Menopause?
Yes, it is. Should you have multiple sex partners, use a condom every time you have sex. If you have only one partner, sex should be just between the two of you. And you both should have an STI test before unprotected sex.
The use of condoms proves to be the best way to prevent STIs. Since a man does not need to release sperm to give or get an STI, ensure you put the condom on before you allow the penis to get to the mouth, vagina, or anus. You may also stand a chance to get STI from unprotected sex. Vaginal dryness or irritation is widespread after menopause and can cause STI to enter through the small tears and cuts.
Contact Us
Contact Gynae Uk if you have any question or need any assistance concerning menopause. You can visit us at South Kensington, London or place a call to us on 02071835411 today.
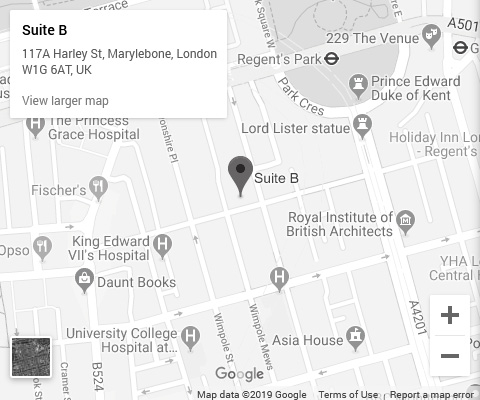 Click To View Full Map
Click To View Full Map
Contact Info
Phone: 020 71835411
Email: info@gynaeuk.com
Address:
20 Old Brompton Road, South Kensington, London SW7 3DL
Opening Hours
| Day | Opening Hours |
|---|---|
| Monday | 9am to 6pm |
| Tuesday | 9am to 8pm |
| Wednesday | 9am to 6pm |
| Thursday | 9am to 8pm |
| Friday | 8am to 5pm |
| Saturday | 10am to 4pm |
| Sunday | Closed |