Located at 20 Old Brompton Road – Just Steps from ![]() South Kensington Tube. Easy Access, Always.
South Kensington Tube. Easy Access, Always.
Fibroids
Fibroids also be referred to as uterine myomas or leiomyomas — they are non-cancerous growths that develop in or around the uterus, often occurring during reproductive years in women. Their growth differs in size and is made up of fibrous and muscle tissues.
Symptoms
The symptoms of fibroids are not typical, and most times, it is diagnosed by chance during a routine gynaecological check-up. Most women are unaware of the growth because there are no visible symptoms. Only 1 in 3 women notice the following symptoms associated with fibroids.
- Abdominal pain
- Frequent urination
- Constipation
- Heavy or painful periods
- Pain or discomfort during sexual intercourse
Even without these symptoms if your GP thinks you have fibroids, you will be referred for an ultrasound scan.
Cause Of Fibroids
The exact cause of fibroids is yet to be discovered, but it has been established that there is a link between the female hormone-oestrogen and fibroids because fibroids usually develop in women during their reproductive years (16 - 50) and decrease as the oestrogen levels become low (menopause).
Oestrogen is the principal female hormone produced by the ovaries. It controls the development of female secondary sex characteristics and reproduction.
Who Can Develop Fibroids?
One in every three women develops fibroids at some point in their life. It is a common condition in women between ages 30 – 50. This condition is said to be prevalent amongst African-Caribbean women and obese or overweight women. Obese women experience the production of high levels of oestrogen in their body. The risk of developing fibroids is quite small in women who have had children and decreases more as a woman gives birth to more children.
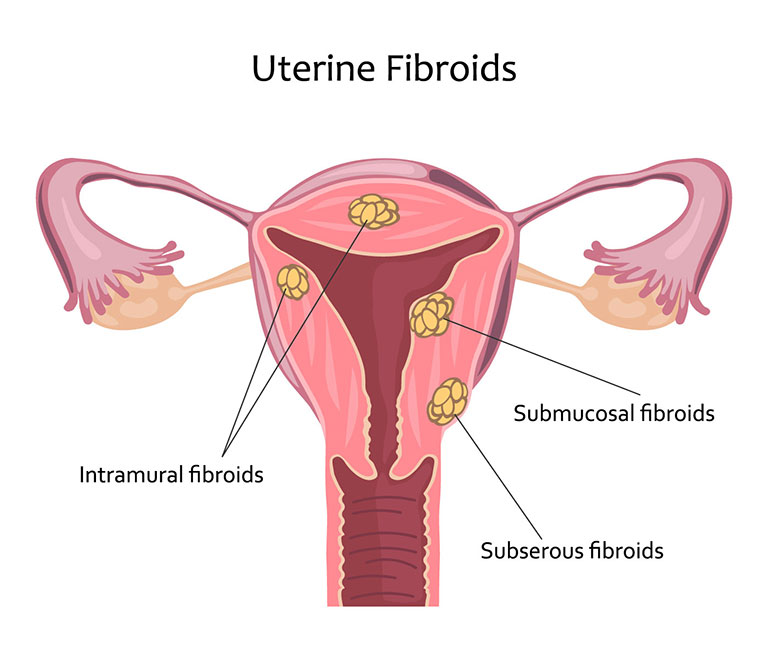
Types Of Fibroids
Fibroids are of different types; it varies in size and the location of the growth. The size of fibroids ranges from that of a pea to the size of a melon.
The main types of fibroids include:
- Intramural fibroids: This is one of the most common types of fibroids, and it develops in the muscle wall of the womb.
- Subserosal Fibroids: This type of fibroids is usually extensive, and it develops outside the walls of the womb into the pelvis.
- Submucosal Fibroids: They develop within the muscle layer that found beneath the inner lining of the womb and grow into the cavity.
- Pedunculated Fibroids: They are subserosal or submucosal fibroids that are attached to the womb with a thin stalk of tissue.
Diagnosis
While some diagnosis of fibroids is conducted during routine gynaecological examinations, there are specific tests carried out in hospitals which your GP may request that you undergo to confirm if you have fibroids and rule out other possible causes of fibroid-related symptoms you may be having. Some of these tests include:
- Ultrasound Scan It is one of the primary investigations carried out to confirm the diagnosis of fibroids. Ultrasound scan is not painful, and it gives off a high-frequency sound wave used to show how the body looks inside. The images obtained from the scan is sent to a monitor where checks for any abnormal appearance or sign of fibroids are conducted. There are two types of ultrasound scan available for the diagnosis of fibroids. They are as follows:
- Abdominal ultrasound scan: For this type of ultrasound scan, the probe that produces the high-frequency sound waves is moved over the outside of the abdomen.
- Transvaginal ultrasound scan: This scan is conducted using a small probe which is inserted into the vagina.
- Hysteroscopy Here your doctor inserts a small special telescope known as hysteroscope into your womb through the vagina opening to examine the inside of the womb — this procedure takes about 5 minutes to be completed. It is used mostly for the check of submucosal fibroids.
During this procedure, your GP may administer a local or general anaesthetic to numb any pain you may feel. Although most women do not need any anaesthetic, a few may experience cramps during the procedure. - Laparoscopy
A small telescope with a camera and light source at its opposite known as a laparoscope is used during this procedure. The camera captures images inside the body and relays them to a monitor.
Laparoscopy is carried out by a surgeon who makes a small incision in the abdomen. The laparoscope is then inserted into the body through the incision to examine the abdomen properly.
The procedure requires the use of a general anaesthetic. It can be used to detect subserosal and intramural fibroids of any size and shape. - Biopsy
This procedure involves taking a small sample of tissue from the womb for a closer examination under a microscope. The tissue sample may be collected during a hysteroscopy or laparoscopy.
Women’s Health is Our Passion
Live life to the fullest with our range of Consultant-led gynaecological services.
BOOK ONLINE NOWTreatment
You may not need treatment for fibroids if there are no symptoms or if the symptoms are mild and do not have any significant effect on your daily activities.
Fibroids can also shrink without medication after menopause and the symptoms usually disappear completely.
In some cases where treatment is required, your GP will either prescribe medications to help relieve the symptoms or shrink the fibroids. If all these medications prove ineffective, then your GP will refer you to a gynaecologist for further help or surgery.
Medications To Relieve Symptoms
Medicines are often made available, but these can be ineffective depending on the size of the fibroids. Many of these drugs are also used to lessen the symptoms of heavy periods. Some drugs available include:
- Levonorgestrel Intrauterine System (LNG-IUS)
An LNG-IUS is a small plastic shaped device placed in the womb. It works by gradually releasing the progestogen hormone known as levonorgestrel — it stops the lining of the womb from overgrowing, therefore, making the womb lining to be thinner and help to reduce bleeding.
Levonorgestrel also functions as a contraceptive, but it does not affect conception once you have stopped using it. Some side effect of this medication includes acne, headaches, tenderness of the breast, irregular bleeding which may last for a period of six months, and also no period in some case. - Tranexamic Acid
Tranexamic acid is a tablet used when LNG-IUS is not suitable, especially cases where contraceptives are not needed.
Tranexamic acid tablet stops the blood vessels in the lining of the womb from bleeding and reduces the loss of blood by 50 %, although it does not affect your chances of getting pregnant in any way.
The tablets are to be taken 3 – 4 times daily during your period. It is advisable to stop the use of Tranexamic acid if the symptoms do not improve within three months. Some side effect of this medication includes indigestion and diarrhoea. - Anti-Inflammatory Medicines
You can take non-steroidal anti-inflammatory drugs (NSAIDs) like mefenamic acid and ibuprofen at least trice daily from the beginning of your period until bleeding eventually stops or reduces.
NSAIDs reduce the production of prostaglandin, a hormone-like substance that is linked to heavy periods and also serves as painkillers — they are not contraceptives, and its possible side effects include indigestion and diarrhoea. - Contraceptive Pills
Using contraceptive pills prevents pregnancy; it stops your ovaries from releasing eggs; it makes bleeding lighter and reduces pain during periods.
Your GP will give you more information about conception and contraceptive pills if you decide to use this form of medication. - Oral Progesterone
Progesterone is a sex hormone in women that helps in the reduction of heaving periods. An oral progestogen is a synthetic form of progesterone — it is a drug taken daily from the 5 - 26 day of your menstrual cycle. Calculations are made using the 1st day of your period as day 1.
Oral progesterone tablets function by preventing the lining of the womb from overgrowing, but it does not serve as a form of contraception, although it can reduce the chances of getting pregnant while taking it. Possible side effect includes weight gain, tenderness of the breast, and short-acne. - Injected Progestogen
Synthetic progesterone is also available as an injection. It reduces heavy periods by preventing the womb lining from overgrowing. Injected progestogen can be administered once every 12 weeks during treatment.
Possible side effects include weight gain, irregular bleeding, absent periods, and premenstrual symptoms like bloating, breast tenderness, and fluid retention.
Injected progestogen can be used as a form of contraception, but it does not prevent conception after you stop using it. However, you may experience up to a 12-month delay before conception.
Medication To Shrink Fibroids
If you still experience fibroid related symptoms while taking any of the symptom reducing medications, then your GP may have to refer you to a gynaecologist and the following medications may be prescribed to help shrink the fibroids.
- Gonadotropin-Releasing Hormone Analogues (GnRHas)
GnRHas like goserelin acetate is injected into the body. It targets the pituitary gland and helps stop the production of oestrogen in the ovaries.
The pituitary gland is small and pea-shaped located at the bottom of the brain — it controls essential hormonal secretions in the body.
GnRHas help reduce pressure in the stomach, relives heavy periods, and stop the menstrual cycle, but they do not affect the chances of conception after you stop using them. It can also be used to prevent frequent urination and constipation. Sometimes, GnRHas are used to reduce the size of fibroids before complete removal with surgery.
Side effects of GnRHas include increased sweating, vaginal dryness, muscle stiffness, hot flushes, and osteoporosis in some cases.
A combination of low doses of hormone replacement therapy (HRT) and GnRHas can be used to prevent all these side effects, and also osteoporosis which is an occasional thinning of the bone can be a side effect. Your GP will prescribe medications to prevent the thinning of your bones and provide more information about this to you.
GnRHas are often prescribed for short term use (a maximum of 6 months). Notably; once you stop taking this medication, the fibroids may grow back to their original size. - Ulipristal Acetate
Your GP may recommend Ulipristal acetate for women over 18 years who are not close to menopause and have the following: - A moderate to severe symptoms of fibroids and are waiting for surgery. In this case, only one course of medication is prescribed.
A moderate to severe symptoms but unable to have surgery. More than a course of medication is often required.
In some cases, Ulipristal acetate causes liver damage. Your GP will ask you to run several blood tests before, during, and after taking this medication to monitor the health of your liver.
Ulipristal acetate is not suitable for women with existing liver conditions because it may increase the chances of having liver damages.
If any of the following symptoms occur while taking this medication, you should contact your GP immediately:
- Nausea or vomiting
- Jaundice
- Itchy skin
- Dark urine
Stomach pain on the upper right side of your body
All these symptoms are also an indication of liver damage.
Surgery
Surgery is considered when the symptoms are severe, and other forms of treatment are not sufficient. There are different surgical procedures available; a gynaecologist will discuss all the options available stating their benefits and risks to you.
The main surgical procedures for the treatment of fibroids are as follows
- Hysterectomy
It is a surgical procedure used to remove the womb, and it is one of the most effective ways of stopping the development of fibroids.
Hysterectomy is usually carried out if you do not wish to have more children, or the fibroids are plentiful, and you are experiencing severe bleeding.
Hysterectomy can be done in different ways, either through the vagina or several small incisions on the abdomen.
The surgeon may use a spinal or epidural anaesthetic to numb the lower part of the body or a general anaesthetic depending on the technique used to carry out the hysterectomy.
When you undergo a hysterectomy procedure, you will need to stay in the hospital for a few days. It should take about 6 – 8 weeks of recovery time, plus you will need to rest for as long as possible. The side effects of hysterectomy include early menopause, and loss of sex drive, especially when the ovaries are removed. - Myomectomy
This is a surgical procedure conducted to remove fibroids from the wall of the womb. It is a better option for women who still want to have children.
Myomectomy cannot be used to remove all types of fibroids. The size, number, and position of the fibroids will determine if myomectomy will be considered.
The size and position of the fibroids also determine the kind of incision that will be made. There may be several small incisions known as keyhole surgery or an open surgery where only a single large incision is made.
Myomectomy requires the use of general anaesthetics and several days stay in the hospital. You will also need to rest for several weeks to fully recover.
Myomectomy is useful in the treatment of fibroids, although there is a possibility that the fibroids may grow back and a need for further surgery. - Hysteroscopic Resection Of Fibroids
In hysteroscopic resection of fibroids, a thin telescope called hysteroscope and small surgical instruments is used to remove the fibroids.
The procedure is used to remove submucosal fibroids in women who still want to have children.
This procedure allows a hysteroscope to be inserted into the vagina through the cervix into the womb, so there is no need for an incision. However, you will need several insertions to remove as much fibroids tissue as possible.
Either general or local anaesthetic can be used, and you will be free to go home the same day you have the procedure.
It is possible to experience stomach cramps and vaginal bleeding after the procedure, but this will subside after a few hours. - Hysteroscopic Morcellation Of Fibroids
This is a new procedure where hysteroscope is used as well as a small surgical instrument to remove the fibroids.
A morcellator is inserted alongside the hysteroscope. It is used to cut and remove the fibroid tissue. A general or spinal anaesthetic can be administered during this procedure, but you will be able to go home the same day after the procedure.
The benefit of hysteroscopic morcellation over hysteroscopic resection is that the hysteroscope is inserted only once, and this reduces the risk of womb injury.
The risks, safety and long-term effect of this procedure is not fully known since it is a new technique.
Non-Surgical Procedures
The non-surgical procedures used in the treatment of fibroids include:
- Uterine Artery Embolisation (UAE)
UAE is used to block the blood vessels that supply blood to the fibroids. It is recommended for women whose fibroids are large. This procedure is carried out by a radiologist (one who is trained to interpret x-rays and scans). During this procedure, a local anaesthetic will be administered before the radiologist injects a small tube called catheter into your leg through a blood vessel.
After the process, you may be required to be in the hospital for about two days, and also 1- 2 weeks of rest before resuming normal activities.
The effect of the UAE on fertility and pregnancy has not been established, but some women still have a successful pregnancy after the procedure.
Notwithstanding, your doctor will discuss all potential risks, benefits and uncertainties with you before this procedure is considered. - Endometrial Ablation
It is a minor procedure used to remove the lining of the womb as a form of treatment for small size fibroids. It can also be used to stop heavy bleeding without fibroids.
The procedure uses several ways to remove the lining of the womb, and it includes:
- Laser energy
- Heated wire lop
Hot fluid in a balloon
This procedure takes about 20 minutes under a local or general anaesthetic to completed, and you will be able to go home the same day.
Vaginal bleeding and tummy cramps may be present for a few days, although some women experience bleeding for up to 4 weeks.
Some women also have severe pain and prolonged pain after the procedure. When this occurs, you should consult your GP.
Getting pregnant after endometrial ablation is possible, but this procedure is not advisable for women who want to conceive because of the increased risk of a miscarriage associated with the process.
- MRI-Guided Procedures
There are two new MRI-related techniques are now available for the treatment of fibroids; they include:
- Percutaneous laser ablation
- Transcutaneous focused ultrasound
These procedures use MRI to guide small needles with laser or ultrasound energy to the centre of the fibroid.
MRI-related procedures cannot be used to treat all kinds of fibroids. The long-term risks and benefits of these procedures are not yet known since they are relatively new and should be taken into consideration. Although some evidence shows that when they are carried out by an experienced clinician, this procedure has short to medium-term benefits.
Complications
In most women, there are no symptoms of fibroids. Still, some significant problems can be observed as a result. Complications also occur depending on factors like the position of the fibroids and their sizes.
Some common complications of fibroid include:
Problems During Pregnancy
Where fibroid is present alongside pregnancy, it can impede the development of the baby and cause further difficulties during labour.
It is conventional for women with fibroids to experience abdominal pain during pregnancy and also to have premature labour.
If the fibroids are large and it blocks the vagina, then a caesarean section may be necessary to deliver your baby. In rare cases, fibroids can also cause miscarriages.
- Infertility
Fibroids can prevent a fertilised egg from attaching to the lining of the womb or prevent sperm from fertilising the egg. Submucosal fibroids that grow from the muscle wall into the womb may block any of the fallopian tubes, making it difficult for a woman to become pregnant.
Contact Us
If you need more information about fibroids, you can visit our gynaecological clinic in South Kensington, London. Or you can place a call to us on 020 7183 5411 today.
 Click To View Full Map
Click To View Full Map
Contact Info
Phone: 020 71835411
Email: info@gynaeuk.com
Address:
20 Old Brompton Road, South Kensington, London SW7 3DL
Opening Hours
| Day | Opening Hours |
|---|---|
| Monday | 9am to 6pm |
| Tuesday | 9am to 8pm |
| Wednesday | 9am to 6pm |
| Thursday | 9am to 8pm |
| Friday | 8am to 5pm |
| Saturday | 10am to 4pm |
| Sunday | Closed |