Women’s health is a vital yet sometimes overlooked part of overall wellbeing. In recent years, there has been a growing awareness in the UK about the importance of addressing women’s health concerns early rather than ignoring them. From conversations around endometriosis to wider screening programmes for cervical cancer, more women are now encouraged to take charge of their gynaecological health.
Gynaecological issues can affect women at every stage of life, from teenage years through to menopause and beyond. Some are relatively minor and easily treated, while others may have long-term consequences if left undiagnosed. The good news is that early detection, timely treatment, and regular check-ups with a qualified gynaecologist can make a world of difference. This article explores the most common gynaecological health issues every woman should know, why they matter, and when to seek professional help.
What Is Gynaecological Health?
Gynaecological health refers to the wellbeing of a woman’s reproductive system, including the uterus, ovaries, fallopian tubes, cervix, and vagina. It also encompasses menstrual health, fertility, and hormonal balance. Maintaining good gynaecological health is essential not only for reproduction but also for overall physical and emotional wellbeing.
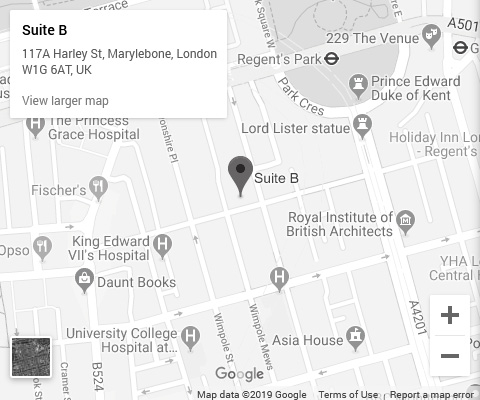
In London, more women are turning to private gynaecologists for personalised and timely care. Unlike routine GP visits, a private gynaecological consultation often provides longer appointment times, faster access to tests, and a tailored approach to individual needs.
A common misconception is that gynaecological care is only necessary during pregnancy or when there’s a serious issue. In reality, regular check-ups can detect problems before they escalate, giving women peace of mind and ensuring early intervention where needed.
Common Gynaecological Health Issues Every Woman Should Know
Menstrual Disorders
Menstrual issues are among the most common reasons women seek gynaecological advice.
- Heavy periods (Menorrhagia): Some women experience excessively heavy bleeding that interferes with daily life, leading to anaemia and fatigue.
- Painful periods (Dysmenorrhoea): While mild discomfort is common, severe cramps that disrupt normal activities could point to conditions such as endometriosis or fibroids.
- Irregular periods: Skipping cycles or experiencing unpredictable bleeding can be linked to hormonal imbalances, stress, or underlying medical conditions.
These problems aren’t just “part of being a woman.” Persistent menstrual issues deserve proper evaluation, especially if they affect work, social life, or fertility.
Polycystic Ovary Syndrome (PCOS)
PCOS is a hormonal condition affecting around 1 in 10 women in the UK.
- What it is: A condition where the ovaries develop multiple small cysts, leading to hormonal imbalances.
- Symptoms: Irregular periods, weight gain, acne, thinning hair, and difficulty conceiving.
- Long-term effects: Increased risk of type 2 diabetes, high cholesterol, and endometrial cancer if left unmanaged.
Women in London often seek private consultations to manage PCOS more effectively through tailored treatment, which may include lifestyle advice, medication, and fertility support.
Endometriosis
Endometriosis affects nearly 1.5 million women in the UK, yet it often takes years to diagnose.
- What it is: A condition where tissue similar to the lining of the womb grows outside the uterus, such as on the ovaries or fallopian tubes.
- Symptoms: Severe pelvic pain, heavy bleeding, pain during sex, and fertility problems.
- Treatment: Options include pain relief, hormonal therapy, and in some cases, surgery.
Raising awareness has encouraged more women to seek early help, particularly as private clinics in London often provide faster access to diagnostic procedures like laparoscopy.
Uterine Fibroids
Fibroids are non-cancerous growths in or around the uterus. They are particularly common in women of reproductive age.
- Symptoms: Heavy or prolonged periods, pelvic pain, frequent urination, and bloating.
- Treatment in the UK: Ranges from medication to shrink fibroids, to surgical options such as myomectomy or hysterectomy. Non-surgical treatments, like uterine artery embolisation, are also available in many London clinics.
Although not usually life-threatening, fibroids can cause significant discomfort and impact fertility, making professional evaluation essential.
Vaginal Infections (Bacterial Vaginosis & Thrush)
Vaginal infections are extremely common and can affect women at any age.
- Causes: Imbalance of bacteria in the vagina, yeast overgrowth, or sexual transmission.
- Symptoms: Unusual discharge, itching, burning, or odour.
- Impact: While usually treatable, recurrent infections can affect sexual health and confidence.
Getting a timely diagnosis is crucial. In London, many private clinics offer same-day testing and treatment, reducing the stress and disruption these conditions can cause.
Cervical Dysplasia and Cervical Cancer
Cervical cancer remains one of the leading causes of cancer in younger women in the UK.
- Prevention: The cervical screening (smear test) programme detects abnormal cells early, significantly lowering cancer risk.
- Symptoms to watch: Unusual bleeding, pelvic pain, or pain during sex.
- HPV vaccination: Now routinely offered to teenagers in the UK, protecting against the high-risk strains of HPV that cause most cervical cancers.
Regular screening, whether via the or private gynaecology services, remains the best protection.
Pelvic Inflammatory Disease (PID)
PID is an infection of the reproductive organs, often caused by untreated sexually transmitted infections.
- Symptoms: Lower abdominal pain, abnormal vaginal discharge, fever, and painful sex.
- Complications: Can lead to infertility, ectopic pregnancy, and chronic pelvic pain if not treated promptly.
- Treatment: Usually involves antibiotics and, in severe cases, hospital care.
Recognising the early warning signs is key. Women should not ignore persistent pelvic pain or abnormal discharge.
When Should You See a Gynaecologist in the UK?
Knowing when to seek professional help can be life-changing. You should book a consultation if you notice:
- Persistent pelvic or abdominal pain
- Unusually heavy or irregular periods
- Unexplained vaginal discharge or bleeding
- Pain during sex or urination
- Concerns about fertility or menopause symptoms
In the UK, women have access to both and private gynaecological services. The provides excellent care but may involve long waiting times. Private clinics, particularly in London, offer quicker access, longer consultation times, and a more personalised approach.
Preventive Measures and Healthy Practices
Prevention is always better than cure. Here are some ways women can maintain good gynaecological health:
- Healthy lifestyle: A balanced diet and regular exercise help regulate hormones and support reproductive health.
- Regular check-ups: Annual gynaecological reviews, even when symptom-free, can detect problems early.
- Safe sexual practices: Using protection reduces the risk of STIs and PID.
- HPV vaccination: Strongly recommended for eligible women and girls, helping to prevent cervical cancer.
Simple steps like these can make a significant difference in maintaining long-term wellbeing.
Conclusion
Gynaecological health is an essential part of every woman’s overall wellbeing, yet it’s often neglected or misunderstood. From common issues like menstrual disorders and vaginal infections to more complex conditions such as PCOS and endometriosis, awareness and early intervention are crucial.
For women in London, access to both and private gynaecology services means there are multiple pathways to care. However, private consultations often provide faster, more personalised attention, which can be invaluable when dealing with time-sensitive concerns.
By prioritising gynaecological health, staying informed, and attending regular check-ups, women can take control of their health and prevent minor concerns from becoming major problems. If you have any symptoms or concerns, don’t wait—book a consultation with a private gynaecology clinic in London and take the first step towards better health and peace of mind.






-in-the-UK.jpg)