Living in London, with its fast-paced lifestyle and endless distractions, it’s easy to overlook subtle changes in your body. But when it comes to your health, being proactive can make all the difference - especially when it comes to conditions like uterine cancer. In the UK, around 9,800 women are diagnosed with uterine (or womb) cancer every year, according to Cancer Research UK. The good news? Early detection significantly improves outcomes. One of the most common early signs is post-menopausal bleeding - a symptom that should never be ignored. Let’s dive into what you need to know about spotting the early warning signs, understanding the causes, and knowing exactly when to seek medical advice.
What Are the Early Symptoms of Uterine Cancer?
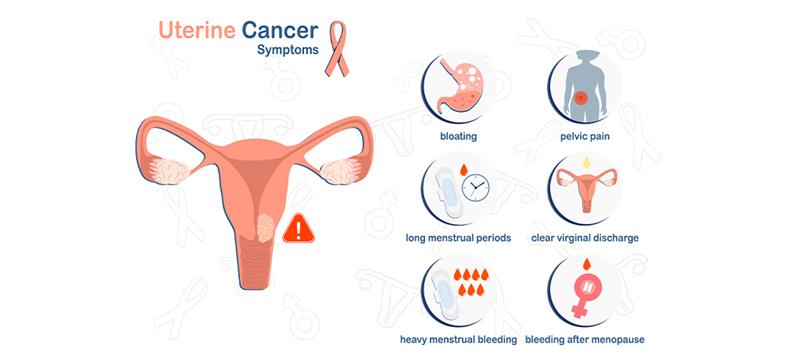
When it comes to uterine cancer, your body often sends signals long before things escalate. Here are some key symptoms to watch for:
- Unusual Vaginal Bleeding
This could mean bleeding between periods if you’re premenopausal or any form of bleeding after menopause. While spotting might seem minor, it’s one of the clearest red flags for uterine cancer. - Heavy or Prolonged Periods
If your periods suddenly become heavier than usual or last longer than they used to, this could indicate something isn’t quite right. - Changes in Vaginal Discharge
Watery, pinkish, or foul-smelling discharge can sometimes signal underlying issues, including endometrial cancer. - Pelvic or Lower Tummy Pain
Persistent discomfort or cramping in your pelvic area may not just be linked to stress or period pain - it could also point to something more serious. - Pain During Sex
If intercourse becomes painful without an obvious reason, it’s worth discussing with your GP.
While these symptoms don’t always mean cancer, ignoring them isn’t an option. Pay attention to what feels out of the ordinary for you.
Post-Menopausal Bleeding: When to See a GP
If you’ve gone through menopause, any vaginal bleeding - no matter how light - is considered abnormal and requires immediate attention. Why? Because post-menopausal bleeding is one of the strongest indicators of uterine cancer.
The advises booking an urgent GP appointment if you experience this symptom. Your GP will likely ask detailed questions about your medical history and conduct an initial examination. Depending on their findings, they may refer you for further tests, such as an ultrasound or biopsy. Remember, catching potential issues early gives you the best chance at successful treatment. Don’t wait until it’s too late; act now.
Risk Factors That Increase the Chance of Uterine Cancer
Understanding your risk factors can help you stay vigilant. Some factors are beyond your control, but others can be managed with lifestyle adjustments. Here’s what increases your chances:
- Age and Menopause: Most cases occur in women aged 50 and above, particularly those who have gone through menopause.
- Obesity and Hormone Imbalance: Excess weight can lead to higher oestrogen levels, which disrupts hormonal balance and raises cancer risk.
- Family History and Genetics: A family history of uterine or colorectal cancer (Lynch syndrome) can increase your susceptibility.
- Hormone Replacement Therapy (HRT) or Tamoxifen Use: These medications can affect hormone levels and potentially raise risks.
- Diabetes and Metabolic Conditions: Insulin resistance and high blood sugar levels are linked to increased cancer risk.
Knowing your personal risk profile empowers you to take preventive measures and seek timely care.
When Abnormal Bleeding Could Mean More Than Period Problems
Not all abnormal bleeding points to cancer. Conditions like fibroids, polyps, or hormonal imbalances can cause similar symptoms. However, distinguishing between harmless and harmful isn’t always straightforward.
For example, spotting between periods might feel alarming, but it could simply be due to stress or birth control changes. On the flip side, persistent or worsening symptoms shouldn’t be brushed off. Keep track of patterns and discuss anything unusual with your GP. They’ll guide you through ruling out benign causes versus investigating more serious concerns.
How Is Uterine Cancer Diagnosed in the UK?
If you visit your GP with suspected uterine cancer symptoms, here’s what typically happens:
- Initial Consultation: Your GP will review your symptoms and medical history and perform a basic pelvic exam.
- Tests: You may be referred for a transvaginal ultrasound to examine the thickness of your uterine lining or a biopsy to collect tissue samples for analysis.
- Two-Week Referral Pathway: If there’s suspicion of cancer, you’ll be fast-tracked under the ’s rapid diagnostic pathway.
Results usually take a few days, and your GP will explain the next steps based on the findings. Whether it’s reassurance or further specialist care, staying informed helps ease anxiety during this process.
Less Common Warning Signs You Shouldn’t Ignore
While bleeding is the hallmark symptom, other less common signs include:
- Persistent Pelvic Pain or Bloating: Often mistaken for digestive issues, ongoing discomfort warrants investigation.
- Unexplained Weight Loss or Fatigue: Sudden drops in weight or constant exhaustion can signal systemic problems.
- Changes in Urination or Bowel Habits: Frequent urges or irregularities might overlap with bladder or bowel conditions but shouldn’t be dismissed.
These symptoms alone might not scream “cancer”, but combined with others, they paint a clearer picture. Always err on the side of caution.
How to Reduce Your Risk of Uterine Cancer
Prevention plays a crucial role in lowering your risk. Here’s how you can take charge:
- Maintain a Healthy Weight: Regular exercise and a balanced diet reduce obesity-related risks.
- Regular Screenings and Check-Ups: Stay up-to-date with routine gynaecological exams, especially if you’re over 50.
- Manage Diabetes and Hormones: Work closely with your healthcare provider to keep metabolic conditions under control.
- Adopt Lifestyle Changes: Quit smoking, limit alcohol intake, and prioritise nutrient-rich foods.
Small, consistent efforts add up to significant benefits over time.
When to Seek Medical Advice in the UK
Here’s the bottom line: if you notice anything unusual - whether it’s unexpected bleeding, pain, or other concerning symptoms - don’t hesitate to book a GP appointment immediately. Early diagnosis saves lives, and thanks to the ’s robust referral system, help is readily accessible. Private clinics in London also offer expedited services if needed.
Your health is worth prioritising, so trust your instincts and speak up. It’s better to address concerns promptly rather than regret waiting later.
Worried About Uterine Cancer?
If you notice unusual symptoms like abnormal bleeding or pelvic pain, book a GP consultation today for timely evaluation. Early detection saves lives.
Conclusion
Uterine cancer might sound daunting, but knowledge truly is power. By familiarising yourself with the early warning signs, understanding risk factors, and seeking timely medical advice, you’re taking vital steps toward safeguarding your well-being.
To recap:
- Be alert to unusual vaginal bleeding, pelvic pain, or discharge changes.
- Post-menopausal bleeding demands urgent GP attention.
- Manage risk factors through healthy habits and regular check-ups.
Remember, subtle signs deserve attention. If you’re concerned about symptoms, consider reaching out to our Private Gynaecology Clinic in London for personalised care. Your body speaks volumes - listen closely, and act wisely.






-in-the-UK.jpg)